Hemorrhoids - a disease associated with inflammation of the varicose veins and swelling of the rectal veins in the anus. Affected areas protrude outward, which can form large knots (bumps) that interfere with the passage and passage of stool. The disease affects men and women, the danger is rupture of the veins, additional secondary infection.
Classification of hemorrhoids
Depending on the location of the pathology, people distinguish two types of diseases:
- Outside. The veins in the anus, which are covered with skin, become inflamed. As a result, it becomes more difficult to destroy the affected areas, they have stronger "protection". Discomfort during defecation is less, but uncomfortable friction from linen is often created. Complications of external hemorrhoids are less common and easier to treat.
- Inland. The affected veins are located in the rectum above the anus, making it difficult to determine the early stage of the disease. Blood vessels are covered with a thin layer of epithelium, so they are more susceptible to mechanical damage. The internal form of the disease often becomes chronic, more dangerous complications, more difficult to treat.
According to the severity of the course, internal hemorrhoids are divided into 3 degrees (stages):
- Initially (1). The lymph nodes are protruding, bleeding but not falling out.
- Moderate (2). With muscle tension (during defecation, movement), swollen veins drain out of the anus. When things relax, they come back.
- Heavy (3). The lymph nodes that fall out, even without muscle tension, do not retract on their own.
Symptom
The main signs of hemorrhoids are bleeding from the anus, pain from straining the muscles of the rectum. The full picture depends on the stage of the disease. If nodes are present (separately swollen veins), they look like a dark pink or purple (rarely nearly black) swelling that is easily palpable and feels dense. The shade depends on the filling of the vessels: if a blood clot has formed, the blood has collected and cannot escape, the nodes will be dark in color.
Internal hemorrhoids
In the first days and weeks, the disease is almost symptomless. It begins with edema, which cannot be felt unless you begin to probe the rectum from the inside. There are no pain receptors in that part, so a person does not feel any discomfort, even during defecation.
In the early stages of hemorrhoids, you can detect its existence only by the drops of blood that appear after passing large, hard stools. Due to edema, the rectal wall narrows the lumen, the mucosa is more damaged when constipated. The important thing - with hemorrhoids, almost every bowel movement will result in a small amount of blood.
Other symptoms will occur as follows:
- Pain during bowel movements. Severe swelling causes muscle spasms, so even soft stools can cause discomfort.
- Burning, itching. Due to inflammation of the rectum, it secretes a lot of mucus, causing irritation to the tissues.
- Blood. It appears in large numbers when nodes are formed. Important: with hemorrhoids it is bright red - not dark.
- release the buttons. Appears in the late stages of hemorrhoids. First, they are attracted to themselves, then they have to be "pushed" with a finger.
Outside
The external veins are covered with skin and contain many pain receptors. Already in the early stages of hemorrhoids, a person will experience discomfort if the vessels are swollen. Pain occurs during defecation, and when wiping the anus and when linen is in close contact with the skin. If the inflammation is severe or a blood clot forms in the vein, a large bump will form. Easy to touch, painful to touch.
The skin affected by external hemorrhoids becomes sensitive, often gathering into folds due to swelling. The process of cleaning the anus after defecation is difficult, so the risk of secondary infections increases. Later, blood will appear if the hemorrhoid is damaged, but less so than when the inner cones form.
Reason
This disease is associated with decreased blood flow in the veins of the rectum, which is usually caused by a blockage of the pelvic organs. Because of them, the pressure in the veins increases, bulges and protrudes. In most people, this happens due to unhealthy lifestyle and nutrition, but doctors do not rule out the influence of genetics, inherited blood vessel defects and increased blood clotting.
Possible reasons for hemorrhoids to appear:
- Frequent constipation - leads to distension of the anal veins, damage to the mucosa during the promotion of solid stools.
- Diarrhea - acute and chronic.
- Pregnancy - causes swelling, which puts pressure from the growing uterus on the rectum.
- Hormonal fluctuations - stimulate the loss of tone of the muscles in the pelvic organs.
- Bowel cancer (more often - colon).
- Postpone operations on the rectum, less often - on the pelvic organs.
- Spinal trauma, scoliosis, lower back injury, sacrum, coccyx.
Additional risk factors:
- Sedentary lifestyle - causes stagnation of blood in the pelvis.
- A low-calorie, low-fiber diet will cause constipation.
- Lifting weights causes muscle tension.
Diagnose
Your doctor will examine your medical history and ask clarifying questions to rule out other causes of anal bleeding. Hemorrhoids have symptoms similar to tumors in the digestive tract, polyps, anal fistula, and mucosal prolapse.
After your doctor performs a rectal exam, feel the lower part of your rectum with your fingers. In the early stages of internal hemorrhoids, this may not work, in later stages, the procedure will be postponed if the swelling is very severe and the patient's touch causes acute pain. To clarify the diagnosis and more detailed examination of the anus, examinations are performed by a surgeon or a gastroenterologist.
The following methods are applied:
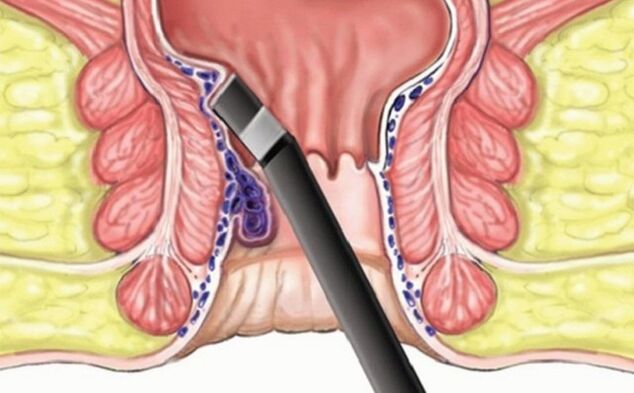
- Endoscopic. Examine a segment of the rectum up to 10 cm long from the anus. The procedure is painless, but some patients receive a local anesthetic (gel, spray).
- Colonoscopy, colonoscopy. A tube is inserted into the patient's colon to rule out other causes of bleeding (tumor) and suspected lesions in the upper part.
- Magnetic resonance imaging. Computed tomography is done if an accurate diagnosis cannot be made based on other procedures.
Research in the laboratory
Blood tests are rarely indicated, it depends on the clinical picture of the disease. This is necessary if a secondary infection is already present to identify the pathogen. They also performed an analysis in situations of heavy bleeding from the rectum to see the hemoglobin level, and the number and activity of red blood cells. Primary diagnosis does not require laboratory procedures.
The treatment
If there are no symptoms of the disease, no special treatment is needed. Your doctor will advise you to change your lifestyle and diet so that hemorrhoids do not grow, stools are softer, and do not damage inflamed, swollen mucous membranes. The patient will be offered more movement, gymnastics aimed at training the muscles of the "hypogastric region" and the small pelvis.
How uncomfortable the hemorrhoid treatment is will be determined by the doctor. In the early stages, medication alone can be controlled. If there are many nodes, they are lumpy and do not come out on their own, surgery may be required. In all of the following situations the patient should follow dietary and lifestyle recommendations, as 50% of the time the disease recurs. The one exception is surgery: subsequently, repeated hemorrhoids occur in only 5% of patients.
Diet
The task of nutrition is to save a person from constipation, to prevent inflammation from developing. Sources of fiber are included in the diet: vegetables, herbs, fresh fruits. Carefully processed grains, especially rice - they can thicken stools. In addition, they drink more pure warm water: it does not allow decomposition, it also accelerates the cleansing of the intestines. Carbohydrates and simple sugars should be eliminated so as not to cause inflammation.
Medical therapy
- Laxative. The composition softens the stool and relieves constipation, preventing new mucosal damage. They are taken orally carefully so as not to cause loss of intestinal muscle tone and diarrhea.
- Candles have anesthetic. Pain relief from internal hemorrhoids.
- Vasoconstrictor drugs. It is also a local therapy that reduces swelling.
- Anticoagulants. Stop bleeding.
- Hormonal preparations. They are used topically (injected) for severe inflammation.
Surgical intervention
In the final stage, hemorrhoids require surgery:
- Cut. An instrument is inserted into the anus, which throws a ring of pus through the knot and tightens it. The affected area disappears after 3-4 days.
- laser surgery. The procedure with minimal trauma, is almost painless, but there are a lot of contraindications to it.
- Classic hemorrhoidectomy. The nodes are removed with a scalpel or a special device, and then "stitched" the edges of the mucosa. If necessary, your doctor will remove the clot during the procedure.
Alternative medicine dose
The early stages of external hemorrhoids include symptomatic treatment:
- Take a warm bath. They are made with calendula, chamomile, sage. These herbs reduce inflammation and muscle spasms. They sit in the tub from 20 minutes to 2-3 times a day.
- Compressor. With mashed raw potatoes, aloe vera juice, chamomile decoction, sea buckthorn oil. They are left on gauze for 30-60 minutes.
Prevent
To avoid the question of how to cure hemorrhoids, follow these simple rules:
- Move more. When sedentary, get up every 1-2 hours for 5-10 minutes. Walk in the fresh air, choose the stairs instead of the elevator, the ability to walk a few meters, without having to drive a car.
- Watch your diet. Eat more plant foods, keep water balance, do not abuse bread and complex carbohydrates - cereals, pasta.

























